Medical device manufacturers face stringent requirements when implementing lazer kesim teknolojisi, where precision tolerances often measure in micrometers and regulatory compliance determines market viability. The integration of laser systems into medical manufacturing demands thorough understanding of FDA guidelines, ISO 13485 standards, and biocompatibility protocols that govern every aspect of production. A single deviation from established parameters can compromise patient safety and trigger costly regulatory investigations that threaten entire product lines.
Önemli Çıkarımlar
Ensure compliance with FDA regulations and ISO 13485 certification for medical device manufacturing quality standards.
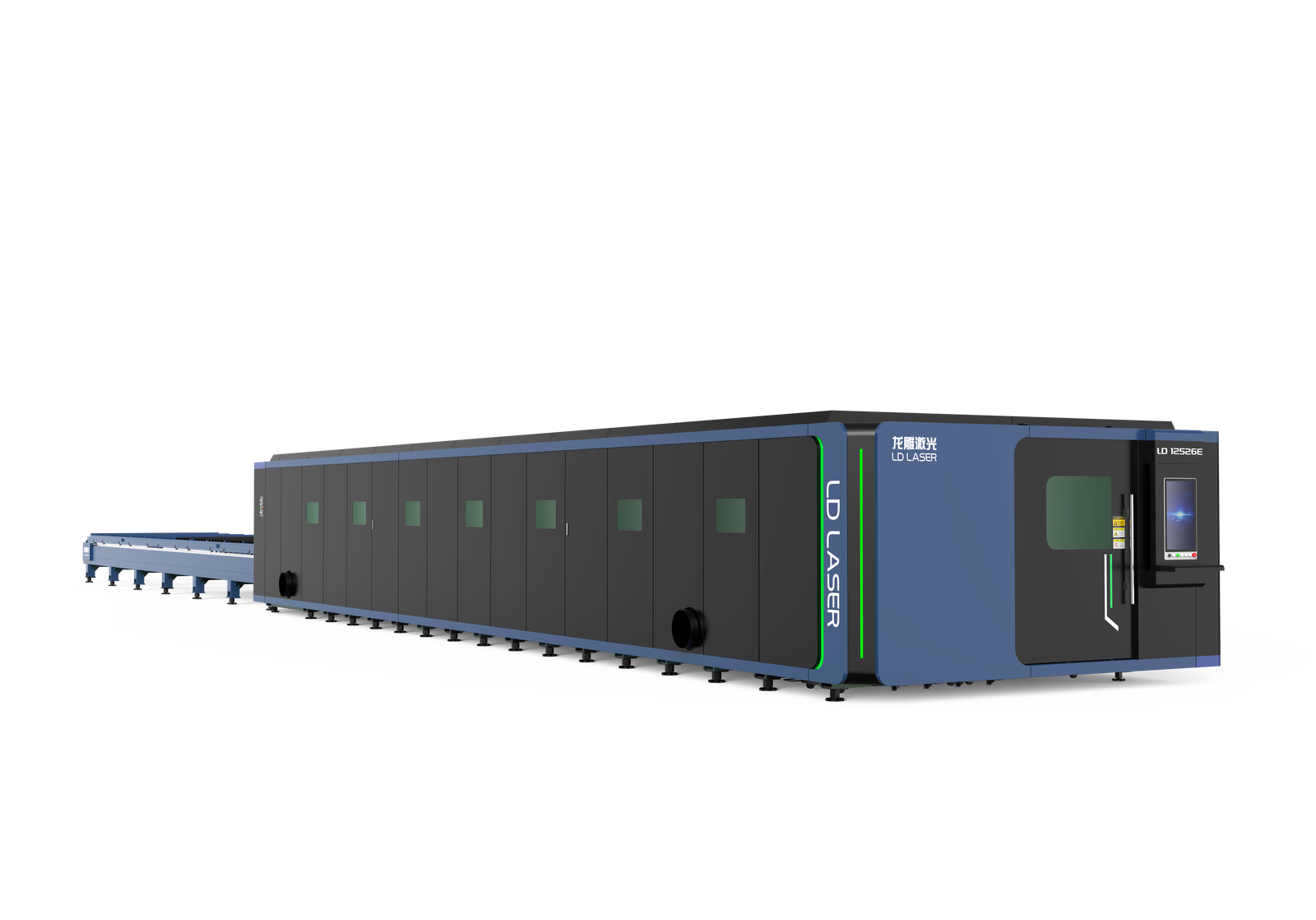
Select appropriate laser technology: CO2 lasers for polymers, fiber lasers for metals based on precision requirements.
Use only FDA-approved, biocompatible materials tested for cytotoxicity in controlled cleanroom environments with HEPA filtration.
Implement continuous quality control with coordinate measuring machines and calibrated laser parameters for consistent results.
Follow strict post-processing protocols including deburring, ultrasonic cleaning, and sterilization for medical-grade components.
Understanding Medical-Grade Laser Cutting Requirements
When implementing lazer kesim teknolojisi in medical applications, manufacturers must navigate a complex landscape of stringent regulatory standards and quality requirements that far exceed those of conventional industrial operations. FDA compliance demands validated processes, thorough documentation, and traceability protocols for every component produced. ISO 13485 certification guarantees quality management systems meet medical device manufacturing standards.
Biocompatibility testing becomes critical when laser-cut materials contact human tissue or bodily fluids. Materials must undergo cytotoxicity, sensitization, and irritation assessments. Clean room environments maintain sterility during production, requiring HEPA filtration and controlled personnel access.
Medical laser innovations continue advancing precision capabilities, enabling intricate geometries in surgical instruments and implantable devices. Laser cutting efficiency directly impacts production costs while maintaining tolerances measured in micrometers. Process validation requires statistical process control, documenting repeatability and reproducibility across production runs. Risk management protocols identify potential failure modes, establishing preventive measures and corrective actions to guarantee patient safety remains paramount.
Selecting the Right Laser Type for Medical Applications
Medical device manufacturers must evaluate laser technology options based on material compatibility and precision specifications required for their specific applications. CO2 lazerler excel at cutting organic materials and polymers commonly used in medical devices, while fiber lazerler provide superior performance for metals and offer enhanced precision for miniaturized components. The selection process requires thorough assessment of cutting tolerances, edge quality standards, and regulatory compliance requirements established by medical device classification standards.
CO2 Vs Fiber Lasers
Selection of the appropriate laser technology represents a critical decision point that directly impacts manufacturing precision, material compatibility, and regulatory compliance içinde medical device production.
CO2 lasers excel in processing non-metallic materials including polymers, ceramics, and composite substrates commonly used in medical applications. CO2 laser advantages include superior edge quality for organic materials, minimal heat-affected zones, and exceptional cutting precision for intricate geometries required in surgical instruments and implantable devices.
Fiber lasers demonstrate superior fiber laser efficiency when processing metallic components, delivering faster cutting speeds and reduced operational costs. Their wavelength characteristics enable precise processing of stainless steel, titanium, and specialized medical alloys while maintaining strict dimensional tolerances.
Material composition, thickness requirements, production volume, and FDA regulatory considerations must guide technology selection to guarantee ideal manufacturing outcomes and patient safety compliance.
Precision Requirements Assessment
Precision tolerances in medical device manufacturing demand systematic evaluation of laser capabilities against specific application requirements. Engineers must assess dimensional accuracy, surface finish quality, and heat-affected zone minimization when selecting appropriate laser systems. Cost analysis encompasses initial equipment investment, operational expenses, and maintenance requirements across different laser technologies.
| Parametre | CO2 Laser | Fiber Laser |
|---|---|---|
| Tolerance Accuracy | ±0.025mm | ±0.010mm |
| Material Compatibility | Polymers, ceramics | Metals, alloys |
| Operating Cost/Hour | $45-65 | $25-35 |
Workflow optimization requires matching laser specifications to production volume and regulatory compliance standards. FDA-regulated applications necessitate validated processes with documented repeatability. Critical assessment factors include beam quality, power stability, and positioning accuracy to guarantee consistent results meeting ISO 13485 requirements for medical device manufacturing.
Material Considerations for Biocompatible Components
Material selection for biocompatible medical components requires strict adherence to FDA-approved specifications and regulatory standards. The chosen materials must demonstrate proven biocompatibility through established testing protocols while maintaining compatibility with required sterilization methods such as gamma radiation, ethylene oxide, or steam autoclave processes. Laser cutting parameters must be optimized for each approved material to prevent contamination, thermal degradation, or alteration of biocompatible properties during the manufacturing process.
FDA Approved Material Selection
Biocompatibility requirements in medical device manufacturing demand rigorous adherence to FDA-approved materials that undergo extensive testing for cytotoxicity, sensitizationve irritation responses. Medical device manufacturers must select biocompatible materials from established databases such as FDA’s recognized consensus standards and ISO 10993 biological evaluation protocols. Common FDA-approved materials include medical-grade stainless steel, titanium alloys, PEEK polymers, and silicone elastomers, each validated through thorough biological testing. FDA regulations require documentation proving material traceability, batch certification, and compliance with specific biocompatibility classifications. Laser cutting operators must verify material certifications before processing, ensuring that thermal effects during cutting do not compromise the material’s biocompatible properties or introduce contaminants that could affect patient safety or regulatory compliance.
Sterilization Compatibility Requirements
When medical devices undergo sterilization processes, the selected materials must demonstrate compatibility with specific sterilization methods including gamma radiation, ethylene oxide (EtO), steam autoclaving, and electron beam sterilization. Laser cutting operators must verify that chosen materials maintain yapısal bütünlük, dimensional stability, and biocompatibility after exposure to these sterilization methods. Certain polymers may experience degradation, discoloration, or molecular chain scission when subjected to high-energy radiation or chemical sterilants.
Material compatibility testing should validate that laser-cut components retain their mechanical properties and surface characteristics post-sterilization. Inadequate material selection increases contamination risks and potential device failure. Documentation must include sterilization validation data and material certificates confirming compatibility with intended sterilization protocols to guarantee regulatory compliance and patient safety.
Setting Up Your Workspace for Medical Device Manufacturing
Establishing a sterile, controlled environment forms the foundation of successful laser cutting operations for medical device manufacturing. The workspace must maintain ISO 14644 cleanroom standards, with HEPA filtration systems removing airborne contaminants that could compromise device integrity. Temperature and humidity controls prevent material expansion and warping during precision cuts.
Workspace ergonomics require strategic placement of laser cutting equipment to minimize operator fatigue and maximize efficiency. Work surfaces should be positioned at appropriate heights, with adequate lighting and clear sight lines to cutting areas. Emergency stop buttons must be easily accessible from all operator positions.
Comprehensive safety protocols mandate proper ventilation systems to extract laser-generated fumes and particulates. Fire suppression systems, laser safety barriers, and personal protective equipment stations are essential components. Material storage areas need segregation between raw materials and finished components to prevent cross-contamination. Documentation stations should be positioned within the controlled environment to maintain regulatory compliance throughout the manufacturing process.
Calibrating Laser Parameters for Precision Medical Parts
Achieving the exacting tolerances required for medical device components demands precise calibration of laser cutting parameters before production begins. Power and speed settings must be systematically adjusted to match material specifications and thickness requirements while maintaining compliance with relevant medical device manufacturing standards. Proper focus positioning and beam alignment serve as critical foundations for consistent cut quality and boyutsal doğruluk across all manufactured parts.
Power and Speed Settings
Calibrating laser power and speed parameters requires meticulous attention to material specifications and dimensional tolerances mandated by medical device standards. Operators must establish baseline cutting parameters through systematic testing protocols, documenting power levels, pulse frequencies, and traverse speeds for each material type. Lower power settings with multiple passes often yield superior edge quality for biocompatible polymers, while titanium alloys require precisely controlled high-power pulses to prevent thermal damage. Speed adjustments directly influence kerf width and heat-affected zones, critical factors in maintaining sterile processing compatibility. Laser safety protocols mandate protective equipment during parameter optimization phases. Documentation of validated settings guarantees repeatability across production runs while maintaining FDA compliance requirements for medical device manufacturing processes.
Focus and Beam Alignment
Precise focal positioning determines the difference between acceptable medical-grade cuts and rejected components that compromise patient safety. Operators must establish ideal focal distance through systematic beam calibration procedures, measuring the beam diameter at various Z-axis positions to identify the smallest focal point. Focus techniques include using calibration plates with graduated thickness measurements and laser power meters to verify beam intensity distribution. Misaligned beams create inconsistent kerf widths, incomplete cuts, and thermal damage that violates FDA manufacturing standards for Class II medical devices. Regular beam calibration protocols require documentation per ISO 13485 quality management requirements. Automated focus systems reduce human error while maintaining repeatability across production runs, ensuring each component meets stringent biocompatibility and dimensional tolerance specifications.
Programming Cut Paths for Complex Medical Geometries
Medical device geometries often feature intricate curves, microscopic tolerances, and multi-dimensional profiles that demand sophisticated programming approaches to achieve regulatory compliance and patient safety standards. Advanced software integration enables operators to translate complex CAD design techniques into precise cutting protocols that maintain dimensional accuracy within FDA-mandated specifications.
Programming these geometries requires strategic path optimization to minimize heat-affected zones and prevent material distortion. CAD design techniques must incorporate lead-in/lead-out sequences, appropriate cutting speeds, and power modulation for varying material thicknesses.
| Geometry Type | Programming Considerations |
|---|---|
| Stent Patterns | Sequential cutting to prevent deformation |
| Catheter Lumens | Controlled perforation spacing |
| Implant Surfaces | Gradual power adjustments |
| Surgical Instruments | Edge quality optimization |
Critical programming parameters include beam compensation algorithms, tool path verification protocols, and real-time monitoring integration. Operators must validate programming outputs through dimensional inspection and material property testing before production implementation.
Quality Control Protocols During the Cutting Process
Bir yandan laser cutting operations proceed, continuous monitoring systems must track critical parameters to assure boyutsal doğruluk and material integrity throughout the production cycle. Real-time sensors monitor beam power, kesme hızı, and gas pressure to maintain consistent cutting accuracy within medical device specifications.
Operators implement inspection methods including coordinate measuring machines (CMM) and optical measurement systems to verify dimensional tolerances during production runs. Statistical process control charts track key variables, enabling immediate corrective actions when parameters drift outside acceptable ranges.
Temperature monitoring prevents thermal distortion in heat-sensitive materials, while particle counters guarantee contamination levels remain below FDA requirements. Documentation protocols require timestamped data collection for every cut piece, creating traceable quality records essential for medical device regulations.
Vision systems automatically detect edge quality defects, burr formation, and kerf width variations. When deviations occur, automated systems halt production and alert quality personnel, preventing non-conforming parts from advancing through manufacturing processes.
Post-Processing Techniques for Medical Components
Following laser cutting operations, medical components undergo essential post-processing procedures to achieve final specifications and regulatory compliance. These techniques guarantee components meet stringent biocompatibility and performance standards required for medical applications.
Deburring represents the primary post-processing step, removing microscopic edge irregularities that could compromise device functionality or patient safety. Operators employ specialized tools including ceramic stones, abrasive brushes, and ultrasonic cleaning systems to eliminate heat-affected zones and surface contaminants.
Material finishing processes follow deburring protocols. Electropolishing enhances surface smoothness for implantable devices, while passivation treatments improve corrosion resistance in stainless steel components. Surface texturing may be applied to promote cellular adhesion in specific applications.
Design optimization considerations influence post-processing selection. Component geometry, intended use, and material properties determine appropriate finishing techniques. Documentation protocols track all post-processing steps, maintaining traceability for regulatory audits and quality assurance verification throughout the manufacturing workflow.
Sterilization and Contamination Prevention Methods
O zamandan beri medical devices must maintain absolute sterility throughout their lifecycle, contamination prevention begins immediately after laser cutting operations and continues through final packaging. Proper sterilization techniques guarantee cut components meet stringent FDA and ISO 13485 requirements while preventing biofilm formation and bacterial adhesion.
Critical contamination controls include immediate transfer to controlled environments following cutting operations. Clean room protocols minimize particulate exposure during handling and inspection phases.
Essential sterilization protocols include:
- Gamma radiation sterilization – Penetrates dense materials effectively while maintaining component integrity at 25-40 kGy doses
- Ethylene oxide (EtO) processing – Compatible with heat-sensitive polymers and complex geometries requiring low-temperature treatment cycles
- Steam autoclave sterilization – Cost-effective method for metallic components using saturated steam at 121-134°C
Validation testing confirms sterility assurance levels meet 10⁻⁶ requirements. Documentation protocols track sterilization parameters, environmental monitoring data, and biological indicator results throughout the manufacturing chain.
Regulatory Compliance and Documentation Standards
Multiple regulatory frameworks govern laser cutting operations içinde tibbi̇ ci̇haz üreti̇mi̇, requiring meticulous documentation systems that demonstrate consistent adherence to quality standards. ISO 13485 mandates extensive quality management systems, while FDA regulations under 21 CFR Part 820 establish specific requirements for device controls and manufacturing processes.
Documentation must include detailed standard operating procedures, equipment calibration records, process validation studies, and operator training certifications. Each laser cutting operation requires traceable batch records documenting parameters such as power settings, cutting speeds, and material specifications. Regular compliance audits verify adherence to established regulatory guidelines and identify potential deviations.
Risk management documentation per ISO 14971 must address laser safety hazards and contamination risks. Change control procedures guarantee any modifications to cutting parameters undergo proper evaluation and approval. Maintenance logs, preventive service records, and equipment qualification documentation provide essential evidence of operational integrity during regulatory inspections and internal quality assessments.
Troubleshooting Common Issues in Medical Laser Cutting
Even with rigorous compliance protocols and documentation systems in place, medical laser cutting operations encounter predictable technical challenges that require systematic diagnostic approaches. Effective troubleshooting techniques guarantee minimal downtime while maintaining sterility and precision standards essential for medical device manufacturing.
Common laser machine errors include:
- Beam quality degradation – Monitor laser power output consistency and inspect optical components for contamination or misalignment, replacing elements according to manufacturer specifications
- Cut quality inconsistencies – Verify material positioning, focus settings, and gas flow rates while checking for mechanical wear in motion systems
- Software calibration drift – Perform routine system diagnostics, update firmware as required, and recalibrate positioning sensors to maintain dimensional accuracy
Operators must document all troubleshooting activities in compliance logs, noting corrective actions taken and verification procedures completed. Preventive maintenance schedules minimize unexpected failures while guaranteeing continued adherence to FDA quality system regulations and ISO 13485 standards.
Maintenance Best Practices for Medical Manufacturing Equipment
Implementing thorough maintenance protocols forms the foundation of reliable medical laser cutting operations, where equipment failures can compromise patient safety and regulatory compliance. Preventive maintenance schedules must align with manufacturer specifications and FDA guidelines, incorporating daily operational checks, weekly component inspections, and monthly detailed evaluations.
Equipment calibration requires precise attention to laser power output, beam alignment, and cutting accuracy using certified measurement tools. Operators should maintain detailed maintenance logs documenting all service activities, calibration results, and component replacements to satisfy audit requirements. Critical components including optical elements, cooling systems, and exhaust filtration demand specialized cleaning procedures using approved solvents and techniques.
Environmental controls must maintain consistent temperature and humidity levels to prevent thermal drift and contamination. Backup systems should undergo regular testing to guarantee seamless shifts during primary equipment maintenance. Qualified technicians must perform major repairs and calibrations, with all work validated through performance verification testing before resuming medical device production.
Sonuç
Medical laser cutting demands meticulous adherence to regulatory frameworks and precision protocols. Operators must maintain sterile environments, document all procedures thoroughly, and guarantee equipment calibration meets stringent standards. Like a medieval scribe recording essential manuscripts, technicians must log every parameter and quality control measure for audit compliance. Regular maintenance schedules, proper material selection, and contamination prevention protocols remain crucial for producing biocompatible components that meet FDA and ISO 13485 requirements in medical device manufacturing operations.